Healthcare providers today face a unique challenge. On one hand, patient care demands their full attention. Conversely, administrative tasks like billing, compliance, and insurance verifications slow them down. It is a balancing act. However, they cannot afford to get it wrong. A trusted medical billing system must do just that in an industry where mistakes are costly – in dollars and loss of a patient’s trust.
Medical billing is a minefield of errors, with Becker’s Hospital Review reporting that nearly 80% of claims contain mistakes. These errors lead to delays in claims processing, denied claims, and ultimately, lost revenues. In healthcare practice, these are not just headaches, but serious threats to financial stability. However, with the right medical billing software, providers can turn these challenges into opportunities.
In this guide, we focus on developing a medical billing system that automates core billing processes but, more importantly, addresses real-world problems. In terms of the content to be covered, we touch everything from core workflows and system integrations to reducing denial rates and ensuring compliance. More importantly, we will show you how a well-built system helps healthcare providers focus less on administration and more on what matters most: patients.
Why medical billing systems matter
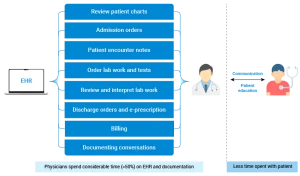
Billing errors and inefficient processes can weaken a healthcare organization. They create bottlenecks, reduce revenue and frustrate patients. The following image highlights the key touchpoints a healthcare organization taps in medical billing. A well-constructed billing system changes that.
A healthcare organization’s routine tasks and responsibilities in medical billing without software assistance.
It ensures faster reimbursements, fewer claim rejections and a smoother overall revenue cycle. Undoubtedly, the following numbers from different estimates speak for themselves:
- U.S. hospitals lose $262 billion each year due to denied claims.
- Manual billing causes a 25-35-day delay in claim payments.
- Medical bills sometimes require 100+ fields to complete.
The numbers above paint a stark picture of the challenges manual medical billing systems face. Here are some more areas where manual touchpoints in a billing system led to inefficiency.
The issues with paper-based medical billing practices
For many years, medical billing was based on manual processes. Naturally, this is both highly inefficient and very cumbersome. For sophisticated health care, this paper-based approach quickly became the largest obstacle to medical practices.
Here are the key issues:
1. High error rates: Humans are fallible. We can make errors in coding, claims verification, or simple data entry. Manual data entry errors occur around 15% of the time. This leads to rejected claims and lost revenues.
2. Time-consuming tasks: There is verification of insurance and the process of denial, which is highly time-consuming. Based on estimates, healthcare providers spend 17 hours a week reworking denied claims.
3. Compliance risks: Billing regulations like HIPAA and ICD coding constantly change. Being manually compliant can lead to costly mistakes that could be considered compliance violations or fines.
4. Delayed payments: The average revenue cycle time in practices reliant on manual billing is 25-35 days. This long wait reduces cash flow, delaying payments and affecting financial health.
5. High operational costs: Maintaining a large billing department to manage manual processes adds to operational expenses. This reduces overall profit margins for healthcare providers.
6. Lack of scalability: As patient volumes grow, manual processes create backlogs. Scaling these outdated systems becomes nearly impossible.
7. Limited data insights: It is not easy to track performance or optimize workflows without automated analytics. Such practices can only take opportunities if they improve billing efficiency and accuracy.
When you look at the bigger picture, it becomes clear: manual processes make it harder to succeed. That is where medical billing software comes in – introducing automation that nullifies the error and maximizes efficiency.
Suggested: A healthcare provider cut manual data entry time by 40% using AI automation. Discover how your billing processes can achieve similar efficiencies. Read about the use cases of generative AI in the healthcare industry.
A step-by-step approach for building a medical billing system
Step 1: Map the core workflows
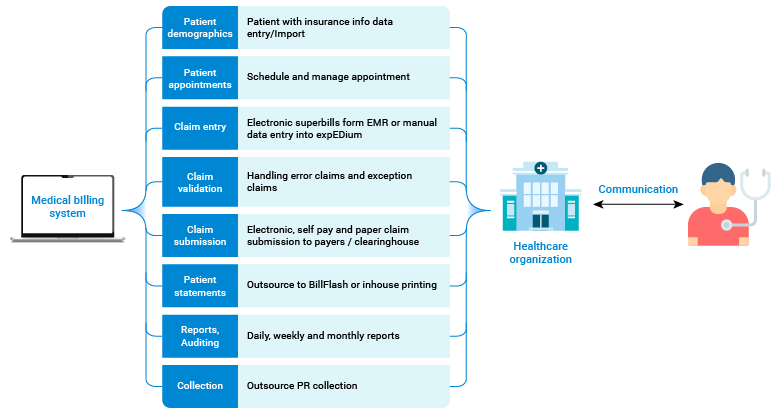
A well-designed medical billing system starts by using core billing workflows. These workflows constitute the heart and soul of the billing cycle, ensuring that the process flows without a hitch from when the patient walks to when the final payment check is cashed. Some of these include the following:
| Workflow | Purpose |
| Patient registration | Capture and validate patient information, including insurance, at first patient contact. |
| Insurance verification | Confirm in real time whether the patient’s policy will cover the treatment they seek. |
| Medical coding and claims | Relate the care to standard code recommendations for the medical providers (ICD and CPT) and make the claims based on the treatments offered. |
| Claims submission | Submit claims electronically to payers or through clearinghouses, reducing processing time and ensuring accuracy. |
| Claims tracking and denial | Track the progress of claims, quickly flag and fix denied claims, and resubmit them efficiently. |
| Payment posting | Log payments from insurers and patients, and ensure accounts reflect up-to-date balances. |
| Patient billing | Generate statements for patients, clearly outlining any outstanding balances, and offer online payment options for ease. |